– Risks for emerging epidemics in the light of accelerating climate change –
E. Elias Hakalehto, PhD, Adj. Prof. (Universities of Helsinki and Eastern Finland)
Microbiologist, Biotechnologist
CEO, Finnoflag Oy
Vice President, International Society of Environmental Indicators
In a typical microbial community, none of its members can be doomed as unnecessary. If a strain is not crucial for the community for the time being, it can be irreplaceable sometimes in the future. The versatility of any mixed population is always the foundation of its essential strength. To survive better, the microbial community has to incessantly diversify and this is in part the explanation for the existence of bacterial viruses or bacteriophages. However, some types of viruses or bacteria may turn out to be hazardous pathogens. Moreover, it is possible that the joint or cumulative effects of various waves of epidemics could lead to a novel situation.
Considering traits such as antibiotic resistance or its markers in the microbial community, we find a cross-cutting issue. The purpose of the antibiotic production is to gain a competitive advantage for the strains producing these agents. However, in a microbial community, it is seldom advantageous for any species to become over-dominating. In the intestines, this leads to dysbiosis and decreased ability of the community to exploit the nutritional resources. Therefore, the interactions in the microbiome are delicate ones. In a pandemic condition, however, the balance of the microbiome may get broken in many cases. The patients, also after the remission, suffer from the consequences of symptomology called “long COVID”. Also, the disturbances in the microbiological balances due to the viral attack and the medications are common phenomena.
The resistance genes in various bacterial strains can be situated in the transposable plasmids or other transferable genetic elements. This means that they can move from one strain to another. Factors carrying the antibiotic resistance could be responsible for the enzyme activities, such as adenylation, acetylation or phosphorylation of the antibiotic. Some antibiotics, such as polymyxin-beta-sulfate, may block the bacterial intake of substances. Other resistance factors may exclude the drug in question from the cell or provide ribosome protection, as is the case with the tetracyclines.
Another example of overcoming an antibiotic resistance is the clavulanic acid. This compound inhibits the enzyme beta-lactamase, which is the resistance factor against penicillin and some related antibiotics. The author was a young microbiologist participating in a biotechnology postgraduate course in London and Canterbury, U.K. in 1984-85, where my task was to construct a chimeric plasmid vector for transferring genes from Streptomycetes to Escherichia coli. The former was the producers for 95% of the antibiotics, whereas the latter was much easier to be used for industrial production by bioengineering solutions. As the vector was constructed, we used it for transferring the clavulanic acid gene into E. coli from Streptomyces clavuligerus. During my studies in England, I participated in lectures and industrial pilot plant training in the University College of London under such scientific leaders and professors as Prof. Malcolm D. Lilly and Prof. Peter Dunnill. The Bioengineering unit is where I learned that contamination might start from a single cell foreign to the process or the body system. University College was also where, some decades earlier, industrial processes for the biotechnical production of antibiotics and enzymes were initiated by some groundbreaking research of the bioengineering groups. The physiology of various microbes and their communities were lectured every Friday at the University of Kent at Canterbury under the supervision of Prof. Alan T. Bull as a part of the biotechnology course.
Today, some 36 years later, there is a great risk of spreading antibiotic-resistant markers in the aftermath of the COVID-19 pandemics. It is generally accepted that viral infections lower the capacity of human immune defences to fight against bacterial illnesses. The viruses also damage the epithelial membranes, thus providing entry for bacteria into the system. After some months of recovery after the COVID-19, most patients are on the antibiotic courses, which indicates the elevated risk for the resistant forms to get disseminated. In fact, during the “Spanish flu” over a century ago, 70% of the deaths associated with that devastating pandemics were associated with bacterial complications by pneumococci, staphylococci and others. If the modern resistant forms get the upper hand now, this could lead the healthcare systems to the brink of collapse.
In India, 13.2% of the population received the first dose of the anti-SARS-CoV2 vaccine by 6th 0f June, 2021. However, as an alarming sign of the potential complications, Mucormycosis (the “black fungus”) has spread among the diseased. This dangerous fungal infection of the respiratory tract has become increasingly abundant due to high SARS-CoV-2 infection rates. Such problems have sometimes occurred also in the water-damaged buildings in Finland and elsewhere. This demonstrates the need to shelter from the conjugated pathogenesis, not against a single causative agent only. At the end of the episode, it might happen that the risk taught to be a secondary one becomes the worst long-term consequence.
One of the most severe bacterial pathogens is Mycobacterium tuberculosis. This bacterium may have caused more deaths in human history than all the other microbial pathogens together. Inactivated M. tuberculosis cells are often used as adjuvants, boosting the immunogenicity of the accompanying other antigens. Such mixture is the Freund´s Complete Adjuvant (FCA), attracting the macrophages and thus yielding better immune responses against the desired antigen in the mixture.
Our laboratory at Finnoflag Oy has speeded up the slow-growing environmental mycobacteria, such as Mycobacterium marinum, in the PMEU device (Portable Microbe Enrichment Unit). 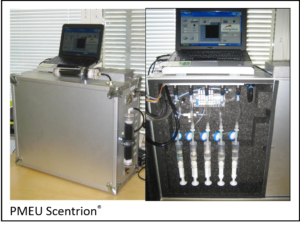 The results of these studies were published in the Pathophysiology Journal in 2013 and 20141,2. The microbial cultures of such slowly propagating bacteria could reach detectable levels, starting from single cells, in days instead of weeks, or hours instead of days. In the PMEU unit, it was also possible to speed up the onset of bacterial growth by leading the carbon dioxide emission from one culture of cells into the other, as described previously by Hakalehto and Hänninen in 2012.3 In fact, the boosting effect of the carbon dioxide may explain the absence of bacterial growth if this gas is totally lacking from the ambient air. Oppositely, we could anticipate that the increase of carbon dioxide could have an accelerating effect on the microbiological degradation processes .
The results of these studies were published in the Pathophysiology Journal in 2013 and 20141,2. The microbial cultures of such slowly propagating bacteria could reach detectable levels, starting from single cells, in days instead of weeks, or hours instead of days. In the PMEU unit, it was also possible to speed up the onset of bacterial growth by leading the carbon dioxide emission from one culture of cells into the other, as described previously by Hakalehto and Hänninen in 2012.3 In fact, the boosting effect of the carbon dioxide may explain the absence of bacterial growth if this gas is totally lacking from the ambient air. Oppositely, we could anticipate that the increase of carbon dioxide could have an accelerating effect on the microbiological degradation processes .
The overall impact of the slightest changes on the partial pressures of the atmospheric gases could be significant from many points of view. We could see the rise in infectious epidemics due to that gradual increase in the content of the atmospheric carbon dioxide, for instance. Considering the mycobacterial pathogens, including the M. tuberculosis bacterium, these strains are often microaerobic ones. The normal partial pressure of oxygen in the alveoli is 104 mmHg, whereas, in the atmospheric air, the corresponding value is 160 mmHg. Consequently, the optimal oxygen concentration for, e.g. M. tuberculosis could theoretically be around 13.65% (instead of 21% in the atmosphere). Please see the “Microbiological Clinical Hygiene”, edited by the undersigned for Nova Science Publishers, Inc., N.Y, for the considerations regarding the mycobacterial and other pulmonary infections4.
Almost one human individual out of four in this world is a carrier (of the Mycobacterium tuberculosis, the causative agent of Tuberculosis (TB). Mycobacteria are prone to increase by the exhaust fumes and increasing carbon dioxide in the atmosphere. As an overall effect of elevated levels of anoxic microbial metabolism, the global degradation processes are also increasing, leading to desertification, unless we could turn the wheel by harnessing micro-organisms for binding atmospheric carbon and nitrogen for the plant culture. This has been envisioned in Tampere, Finland, where my company Finnoflag Oy was the key technology provider. In their “Zero waste from zero fibre” project funded by the Finnish Ministry of Agriculture and Forestry during 2018-19, we demonstrated the total conversion of environmental sediments from the lake Näsijärvi bottom into useful products, such as lactate and other valuable chemicals, energy gases methane and hydrogen, and organic fertilizers. Moreover, as an example of ecosystem engineering, the Tampere project was anticipated to provide a method to remove the pollution from the water environment where it had accumulated during the operations of century-long exhaustion of forest industry wastes. The future of this would be the turning point of using microbes to compensate for climate change in the hands of local politicians.
In the first place, TB patients are treated with primary antibiotics such as isoniazid, rifampicin or fluoroquinolones. Basic level multi-resistance is related to the lack of response to the two first mentioned ones. The outcome of the TB disease may also result from reduced personal immunity, which can follow, e.g. difficult viral infections, such as SARS-CoV-2. Therefore, there is a potent risk of the multi-resistant TB forms to initiate new emerging pandemics. In case of the need for rapid means for effectively preventing both new viral pandemics and the antibiotic-resistant bacterial complications in their aftermath, please see my recent article about the chicken IgY antibodies and the COVID-19 in the IMAJ Journal.5
There are solutions for dealing with the multi-resistant forms of M. tuberculosis, such as MDR-TB and XDR-TB. These include tough treatments (up to two years) with second-line antibiotics, fluoroquinolones and aminoglycosides. Moreover, the speeded-up enrichment and detection with the PMEU units could facilitate earlier and faster treatments. In the hospital setting, the UV-C light could eradicate two-thirds of the tuberculosis-causing bacteria. This surface purification and air decontamination method could be combined with other disinfection protocols. Most importantly, any routes for the contagion by multiresistant strains should be revealed and confined to protect the patients, clinical premises, and outpatients.
References:
1- Hakalehto E. Enhanced mycobacterial diagnostics in liquid medium by microaerobic bubble flow in Portable Microbe Enrichment Unit. Pathophysiology. 2013 Jun;20(3):177-80. doi: 10.1016/j.pathophys.2013.08.005. Epub 2013 Sep 25. PMID: 24075064.
2- Hakalehto E, Heitto A, Heitto L, Rissanen K, Pesola I, Pesola J. Enhanced recovery, enrichment and detection of Mycobacterium marinum with the Portable Microbe Enrichment Unit (PMEU). Pathophysiology. 2014 Sep;21(3):231-5. doi: 10.1016/j.pathophys.2014.07.005. Epub 2014 Aug 4. PMID: 25156813.
3- Hakalehto E, Hänninen O. Gaseous CO2 signal initiates growth of butyric-acid-producing Clostridium butyricum in both pure culture and mixed cultures with Lactobacillus brevis. Can J Microbiol. 2012 Jul;58(7):928-31. doi: 10.1139/w2012-059. Epub 2012 Jun 14. PMID: 22697044
4- Hakalehto E. (Editor): Microbiological Clinical Hygiene (Microbiological Hygiene) 1st Edition – Nova Science Pub Inc; 1st edition (January 15, 2015), ISBN-10 : 1634634284
5- Hakalehto E. Chicken IgY Antibodies Provide Mucosal Barrier against SARS-CoV-2 Virus and Other Pathogens. Isr Med Assoc J. 2021 Apr;23(4):208-211. PMID: 33899350.
Copyright Elias Hakalehto and Finnoflag Oy
Published on 8th of June, 2021
Edited by Dr. Vladimir Jakovljevic (Microbiome Power)